In the relentless pursuit of effective treatments for neurodegenerative diseases, scientists have turned their attention to an innovative approach that targets the very powerhouses of our cells - the mitochondria. Mitochondrial transplantation, a groundbreaking therapeutic strategy, is emerging as a beacon of hope for conditions like Alzheimer's, Parkinson's, and ALS that have long eluded definitive cures.
The concept might sound like science fiction, but researchers are demonstrating that replacing damaged mitochondria with healthy ones could potentially halt or even reverse the progression of these devastating neurological disorders. This approach represents a paradigm shift from traditional treatments that merely address symptoms rather than the underlying cellular dysfunction.
Understanding the Mitochondrial Connection
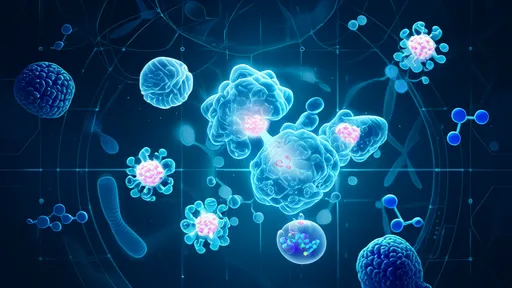
Mitochondria, often described as the cell's batteries, play a crucial role in energy production and overall cellular health. In neurons, these organelles are particularly vital due to the brain's enormous energy demands. When mitochondria malfunction, neurons starve and eventually die, leading to the characteristic symptoms of neurodegenerative diseases.
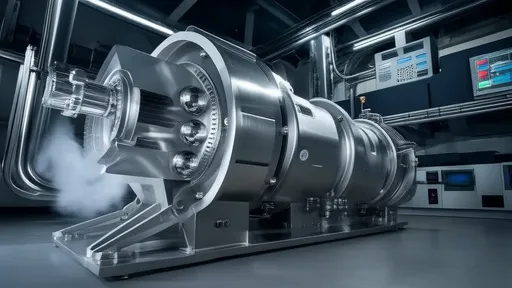
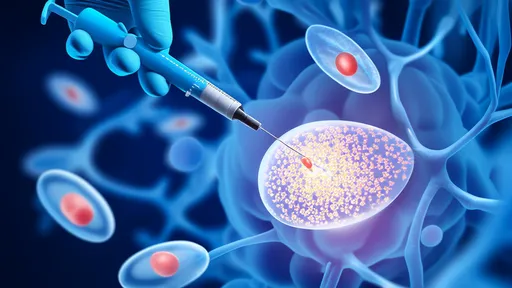
Recent studies have revealed that mitochondrial dysfunction appears early in the disease process, often before noticeable symptoms emerge. This discovery has fueled interest in mitochondrial transplantation as a potential way to intervene before irreversible damage occurs. The technique involves extracting healthy mitochondria from donor cells and delivering them to affected neurons, essentially giving cells a new lease on life.
From Laboratory to Clinical Potential
The journey of mitochondrial transplantation from bench to bedside has been both exciting and challenging. Early experiments in cell cultures and animal models have shown remarkable promise. In Parkinson's disease models, for instance, transplanted mitochondria have been observed integrating into neurons and restoring energy production, leading to measurable improvements in motor function.
One particularly compelling study demonstrated that mitochondrial transplantation could reduce the accumulation of toxic protein aggregates - a hallmark of many neurodegenerative diseases. The healthy mitochondria appeared to enhance the cell's ability to clear these harmful proteins, suggesting the therapy might address multiple pathological processes simultaneously.
Delivery Methods: Crossing the Blood-Brain Barrier
A significant hurdle in developing this therapy has been finding effective ways to deliver mitochondria to the brain. The blood-brain barrier, while essential for protecting the central nervous system, presents a formidable obstacle for therapeutic interventions. Researchers are exploring several innovative delivery methods, including intranasal administration and direct injection into cerebrospinal fluid.
Some of the most promising approaches involve using stem cells as mitochondrial donors or developing specialized nanoparticles to transport mitochondria across the barrier. These delivery systems not only protect the mitochondria during transit but also help target them specifically to affected brain regions, increasing the therapy's precision and effectiveness.
Safety and Ethical Considerations
As with any novel medical intervention, mitochondrial transplantation raises important safety and ethical questions. Scientists are carefully investigating potential risks, such as immune reactions to transplanted mitochondria or unintended effects on cellular function. Early clinical observations suggest that autologous transplantation (using the patient's own mitochondria) may minimize rejection risks.
The ethical landscape is particularly interesting when considering the source of donor mitochondria. While using a patient's own cells is straightforward, allogeneic transplantation (using donor mitochondria from another person) introduces complex questions about cellular identity and long-term effects. Ongoing research aims to establish clear guidelines for these scenarios.
Clinical Trials and Future Directions
The first wave of clinical trials exploring mitochondrial transplantation for neurodegenerative diseases is already underway. Preliminary results from small-scale studies have been cautiously optimistic, showing good tolerability and hints of clinical benefit. Larger trials are now being designed to rigorously evaluate efficacy across different stages of disease progression.
Looking ahead, researchers envision combining mitochondrial transplantation with other emerging therapies, such as gene editing or neuroprotective drugs, to create comprehensive treatment regimens. There's also growing interest in developing mitochondrial banking systems, similar to cord blood banking, to ensure timely access to high-quality mitochondria for therapeutic use.
Challenges and Limitations
Despite the enthusiasm surrounding this approach, significant challenges remain. The complexity of neurodegenerative diseases means that mitochondrial dysfunction is just one piece of a larger puzzle. Questions persist about how transplanted mitochondria will behave in the long term and whether they can truly integrate into the complex neural networks of the human brain.
Another critical issue is timing - researchers are working to determine the optimal stage of disease progression for intervention. Early treatment might offer the best chance of preventing damage, but diagnosing neurodegenerative diseases in their initial phases remains difficult. Developing reliable biomarkers will be crucial for identifying candidates who could benefit most from mitochondrial transplantation.
A New Era in Neurology
As the field of mitochondrial medicine continues to evolve, its potential applications extend beyond neurodegenerative diseases. Conditions ranging from metabolic disorders to cardiovascular diseases and even aging itself might benefit from mitochondrial therapies. This convergence of neurology, cell biology, and regenerative medicine represents one of the most exciting frontiers in modern healthcare.
For patients and families affected by neurodegenerative diseases, mitochondrial transplantation offers something precious that has been in short supply - genuine hope. While much work remains before this approach becomes standard care, the rapid progress in research suggests we may be witnessing the dawn of a new therapeutic era.
The coming years will be critical for determining whether mitochondrial transplantation can fulfill its promise. What's certain is that this innovative approach has already changed how scientists think about treating neurodegenerative diseases, shifting the focus from managing symptoms to potentially restoring cellular health at its most fundamental level.
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025

By /Jul 9, 2025

By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025
By /Jul 9, 2025
By /Jul 9, 2025

By /Jul 9, 2025